Scabbard Research, Inc.
innovators of medical and dental products.
Reprinted from the Journal of Prosthetic Dentistry, Vol 49:546, 1983
Editor's note:M. F. Levenson presents a simple way to alleviate or prevent pain associated with mandibular force necessitated by orthopedic care. The technique and rationale for care should be useful to those dealing with this situation, especially auxiliaries. This article describes a simple, auxiliary-oriented, preventive therapy for the pain associated with mandibular forces involved in orthopedic therapy. G. J. C.
Relieving Intraoral Pressures Generated During Orthopedic Treatment
M. F. Levenson, D.D.S.
- Assistant Clinical Professor, Department of Pedodontics; Dental Director, University Youth Spine Center
- Case Western Reserve University, School of Dentistry, Cleveland, Ohio
Approximately 20% of patients undergoing orthopedic therapy complain of "pain in the jaws." Orthopedic treatment may generate compressive forces on the teeth and jaws that can initiate this "pressure pain syndrome" in the maxillofacial structures. These forces result from constant direct pressure on the mandible during orthopedic treatments with traction body casts and braces.1 These forces are applied in a longitudinal fashion either up to the voluntary tolerance of the patient or in passive stretching at lower pressures.
Therapy related to correction of spinal curves is based frequently on the action and reaction of forces of significant magnitude. At times this force can reach 20 pounds of longitudinal traction across the spine as indicated with strain gauges and pressure cell monitoring.'
The forces on the mandible and resultant intruding occlusal forces produce pain in the apical regions of the premolars and molars. The pain, usually bilateral, is more marked in the mandibular regions. It occurs without temporomandibular joint (TMJ) symptoms, extreme tooth mobility, or pain or thermal hypersensitivity in the teeth.
The symptoms usually subside in 2 to 3 weeks if untreated. However, if the painful stimuli can be prevented or treated, the primary orthopedic therapy can be completed more comfortably. This report describes a simple device that has been effective in reducing the pain.
THE INTRAORAL CUSHION
Patients can be treated successfully with an intraoral cushion (IOC) to relieve trauma to the teeth and supporting structures. The IOC supplies a pressure-absorbing medium between the teeth to diffuse the noxious pressure.
Making the device is simple. An arch form is cut from a thermoplastic polyvinyl sheet (generic thermoplastic polyvinyl sheets are available) approximately 3 to 5 mm thick.
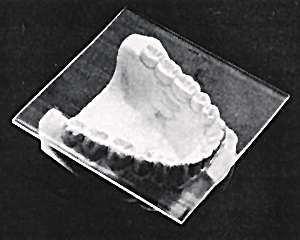
Sheet of resilient material is placed over lower arch prior to cutting to size and shape. Diagnostic casts are not necessary.
|
The IOC is fitted and adjusted best with the patient present unless diagnostic casts have been made previously, in which case the device may be constructed in the laboratory. After the polyvinyl sheet is cut roughly to size, it is softened by heating, tempered in hot water, and inserted in the mouth. The canine notch serves to orient the form. Patients are asked to close their mouth firmly into the sheet. When the material has cooled to the point of relative stability, it is removed from the mouth. If cuspal indentations are not deep enough to permit definite positioning and retention, the sheet is reheated, tempered, and reinserted. Overextensions are trimmed with scissors.

Intraoral cushion has been trimmed.
Canine notch is used for orientation.
|
Polishing of the device is not necessary. For strength, the borders of the IOC should be extended buccally, lingually, and distally at least 2 to 3 mm.
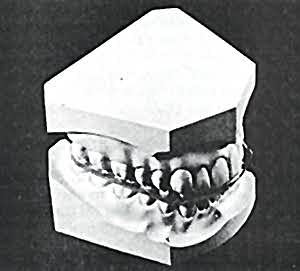
Intraoral cushion simulates its position in patient's mouth
|
Patients are advised to wear the IOC as long as they feel the need for it. The IOC may be fabricated on the cast by dental auxiliaries or hospital staff nurses after they have received brief instructions.
DISCUSSION
Pain in the jaws (pressure pain syndrome) during the early phases of orthopedic treatment has been treated successfully with the IOC system. Apparently some patients undergoing spinal treatment who are free of the pressure pain syndrome voluntarily disengage their teeth or are able to adapt to a low level of discomfort.
The pressure pain syndrome should not be confused with TMJ problems. The signs, symptoms, and treatment are different 3 and the differential diagnosis of the TMJ syndrome is well set forth in a practical manner by Dawson.4 The primary differences are related to the anatomic areas of pain and the case history of the patient. The following TMJ dysfunction signs and symptoms are not part of the pressure pain syndrome: tenderness in the muscles of the jaw, head, and neck; painful TMJs; limited mandibular movements; joint noises; facial deformities; headaches; neckaches; and toothaches. The following signs and symptoms are characteristic of the pressure pain syndrome: pain in the apical region of the maxillary and mandibular premolars and molars; slight mobility of posterior teeth; and pain in second premolars-first molar region following traction and chewing. The design of the IOC resembles that of mandibular repositioning devices used to treat TMJ disorders. However, cushioning the teeth and diffusing the occlusal forces, as opposed to repositioning the mandible, are the reasons for using the IOC to relieve the pressure pain syndrome. The IOC is much more simple than TMJ devices, and it may be constructed by an auxiliary when diagnostic casts are available.
The pressure pain syndrome may result in bone loss. The reaction of bone to pressure has been discussed at length by Weinmann and Sacher.5 They report that pressure on bone results in compression of the periosteal blood vessels and possible crushing and necrosis of the connective tissue adjacent to the bone. Although bone under such pressure may necrotize to a variable depth, its resorption may be retarded. Mobilization of osteoclasts occurs only from the deeper reserves of cellular elements, haversian canals, or marrow spaces. Necrotic bone is removed finally by undermining or retrograde resorption. The extent of bone loss is a function of the reduction of blood supply, which is related directly to the pressure. When physical pressure diminishes or destroys the blood supply of bone or interferes with its venous drainage, the inevitable result is bone resorption. A future study will attempt to measure the extent of this bone loss in laboratory animals, along with the newer techniques of spinal instrumentation.6
Ramfjord and Ash7 state that chewing forces do not exceed 4.5 to 7 kg, and rarely exceed 1 kg. They report that maximum forces in axial and horizontal directions occur in many instances about 20 msec before maximum intercuspation. Axial and lateral occlusal forces persist into the occlusal contact phase and then diminish gradually. Forces up to 100 g can readily displace a tooth. Forces beyond this level and up to 1.5 kg may produce pain. Less tooth displacement occurs if force is applied rapidly. When force is removed, the crown does not return immediately to its original position but does so after I or 2 minutes. As an indicator of the hydraulic forces involved, a number of investigators have reported pulsation of the teeth that has been found to be synchronous with the heartbeat. When sufficient force is supplied to a tooth, distortion of the labial and lingual alveolar plates of bone occurs and suggests other possible physical effects.
The IOC functions primarily as a pressure-dispersing cushion. Its positive effects are not related to an increase in the vertical dimension of occlusion or other actions produced by TMJ dysfunction treatment.
ACKNOWLEDGMENTS
I am indebted to Eleanor M. Brower, R.N., and to Clyde L. Nash, Jr. M.D., Director of the University Youth Spine Center, affiliated with Case Western Reserve University, School of Medicine, and the University Hospitals of Cleveland. I also thank my daughter, Freda Levenson, for her suggestions and help.
REFERENCES
1. Edmondson, A. S., and Crenshaw, A. H., editors: Campbell's Operative Orthopaedics, ed 6. St. Louis, 1980, The C.V. Mosby Co., vol 2, p 1839.
2. Micheli, L., Magin, M., and Rouvales, R.: The patient with scoliosis. Am J Nurs, September 1979, p 1601.
3. Weinberg, L. A., and Lager, L. A.: Clinical report on the etiology and diagnosis of TMJ dysfunction pain syndrome. J PROSTHET DENT 44:642, 1980.
4. Dawson, P. E.: Evaluation, Diagnosis, and Treatment of Occlusal Problems. St. Louis, 1974, The C. V. Mosby Co., p 16.
5. Weinmann, J. P., and Sicher, H.: Bone and Bones. Fundamentals of Bone Biology, ed 2. St. Louis, 1955, The C.V. Mosby Co., p 136.
6. Ferguson, R. L., and Allen, Jr., B. L.: Segmental spinal instrumentation for routine scoliotic curve. Contemp Orthop 2:450, 1980.
7. Ramfjord, S., and Ash, M.: Periodontology and Periodontics. Philadelphia, 1979, W. B. Saunders Co.
Please email us for reprint requests.